CVS HEALTH (CVS)·Q4 2025 Earnings Summary
CVS Health Beats on Revenue and EPS, But Stock Falls 5% on Cash Flow Cut
February 10, 2026 · by Fintool AI Agent
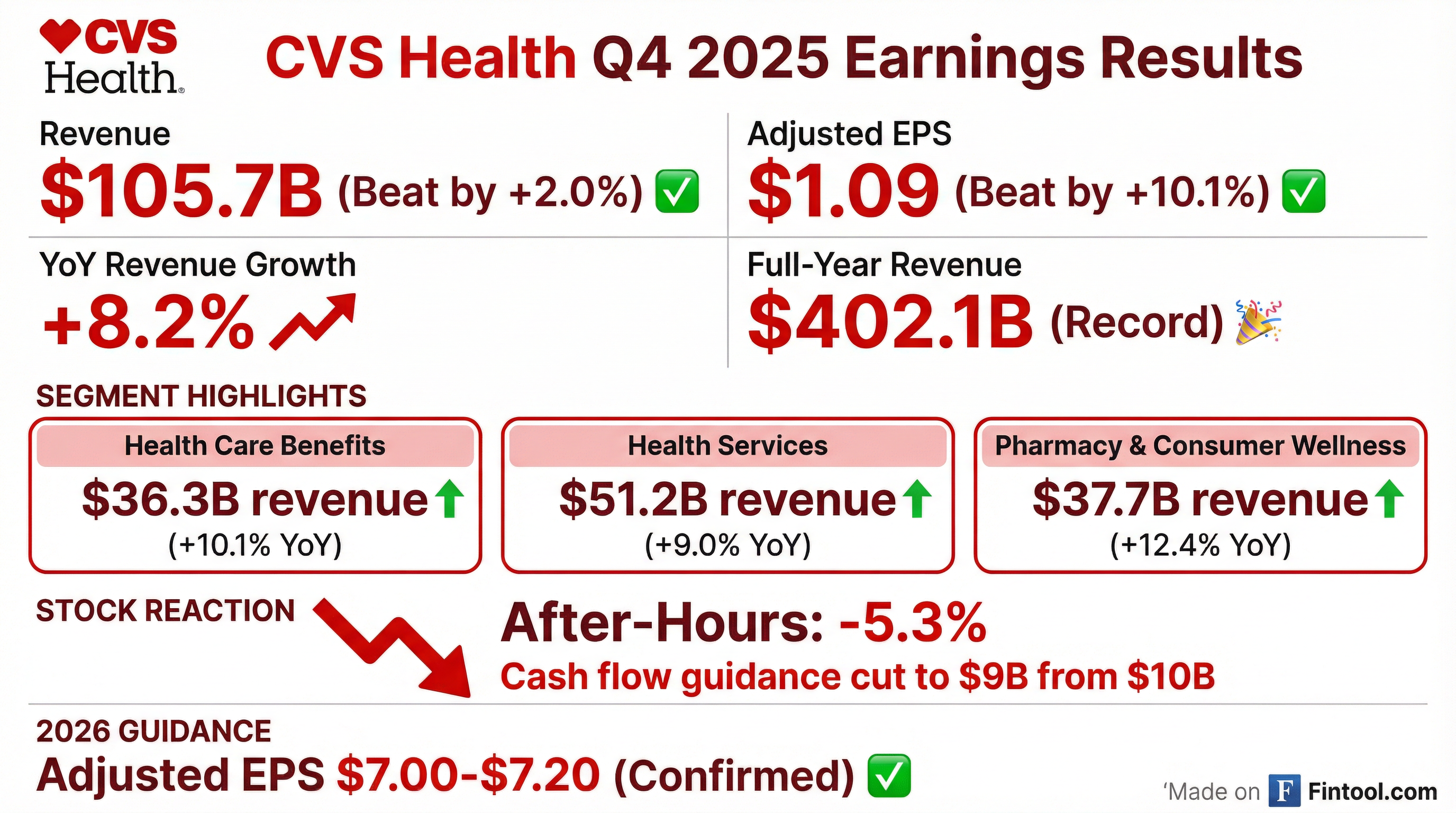
CVS Health delivered a double beat in Q4 2025, with revenue of $105.7 billion (+8.2% YoY) exceeding estimates by 2.0% and adjusted EPS of $1.09 topping expectations by 10 cents . Despite the solid operational performance, shares fell over 5% in after-hours trading after the company cut its 2026 cash flow from operations guidance to "at least $9.0 billion" from "at least $10.0 billion" .
Full-year 2025 revenue reached a record $402.1 billion (+7.8% YoY), with adjusted EPS of $6.75 representing a 24.5% increase from the prior year . CEO David Joyner highlighted the company's transformation progress, stating the company is "well positioned to achieve our ambition to be the most trusted health care company in America" .
Did CVS Beat Earnings?
Yes — CVS beat on both revenue and EPS.
The GAAP EPS of $2.30 was inflated by a ~$1.9 billion tax benefit from a worthless stock deduction related to a subsidiary bankruptcy . Adjusted EPS strips out this one-time item.
Notably, adjusted EPS of $1.09 declined 8.4% from $1.19 in Q4 2024, primarily due to changes in Medicare Part D seasonality under the Inflation Reduction Act (IRA) .
How Did the Stock React?
CVS shares fell sharply despite the operational beat:
The selloff was driven by the cash flow guidance cut and ongoing concerns about Health Care Benefits profitability in Q4 .
What Did Management Guide?
2026 guidance was confirmed, but cash flow outlook was reduced.
The $1 billion reduction in cash flow guidance was the primary driver of the negative stock reaction. However, CFO Brian Newman explained that certain payments shifted from 2026 into late 2025 — meaning the cumulative cash flow expectation across 2025 and 2026 has actually increased by over $1.5 billion .
The FY 2026 adjusted EPS guidance of $7.00-$7.20 implies 4-7% growth from FY 2025's $6.75 .
What About the 2027 Medicare Advantage Rates?
The 2027 Advanced Rate Notice was a major topic on the earnings call — and management was candid about their disappointment.
The proposed rates "simply do not match the level of medical cost trend in the industry," according to CEO David Joyner . CVS is advocating for more appropriate funding to ensure program sustainability.
Key takeaways from management:
Steve Nelson, leading the Aetna business, emphasized that despite the rate notice, the business is "well positioned" with a strong foundation built over 18 months . He noted the team has already engaged with CMS and expects to continue advocacy efforts ahead of the final rate notice.
Oak Street Health Impact: Dr. Shri Narayanan noted that while in-home visits are maintained, "the proposed rates fail to match utilization-to-cost trends, particularly as member needs become more complex." The healthcare delivery business has "clear line of sight to improved performance" in 2026 .
What Changed From Last Quarter?
Key sequential developments:
The Medical Benefit Ratio (MBR) in Health Care Benefits increased to 94.8% in Q4, consistent with Q4 2024, reflecting the IRA's impact on Medicare Part D seasonality .
Days claims payable dropped significantly to 38.9 days from 42.5 days in Q3, indicating faster claims processing .
How Did Segments Perform?
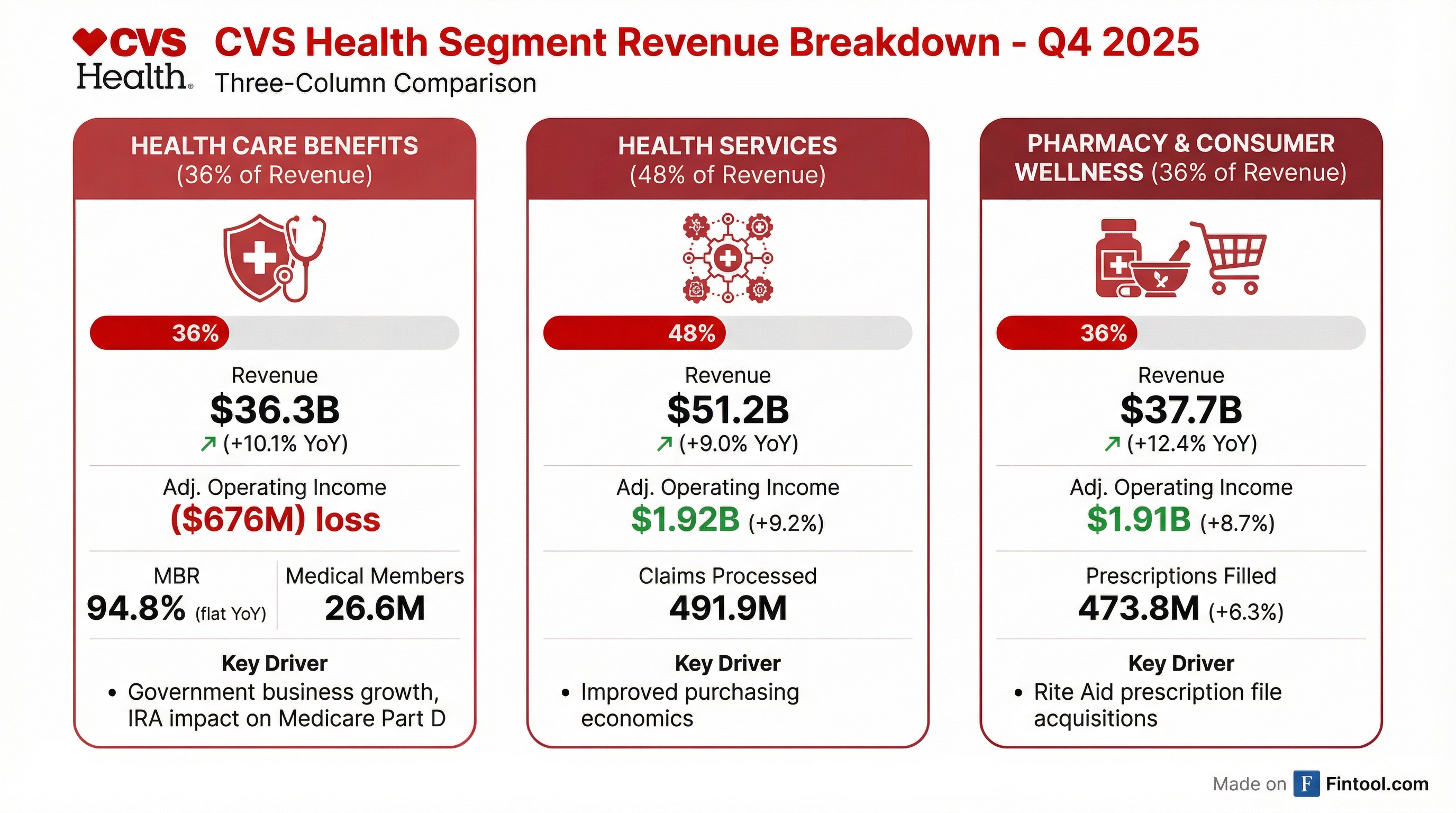
Health Care Benefits
The segment posted an operating loss of $676 million, worse than the $439 million loss in Q4 2024. This was driven by IRA-related Medicare Part D seasonality changes and unfavorable premium deficiency reserves .
For the full year, however, adjusted operating income improved dramatically to $2.9 billion from just $307 million in 2024, driven by improved Government business performance .
Health Services
Revenue growth was driven by pharmacy drug mix and brand inflation, partially offset by client price improvements . The segment's Caremark PBM business "closes out 2025 with significant customer wins and strong retention" .
Pharmacy & Consumer Wellness
The strongest segment performance was driven by Rite Aid prescription file acquisitions and favorable drug mix . Same-store prescription volume grew 9.7% on a 30-day equivalent basis .
CVS Pharmacy "successfully completed the transition to cost-based reimbursement" across all its major businesses .
Key Management Quotes
"I'm proud of our progress strengthening our operations and driving improved financial performance... We still have an incredible amount of earnings power to unlock across our diversified business."
— David Joyner, Chair and CEO
"We have built a competitive advantage that we believe no one else in healthcare can replicate."
— Prem Shah, EVP & Chief Pharmacy Officer
Operational highlights emphasized by management:
- Aetna approving >95% of prior authorizations within 24 hours, with many completed instantaneously
- CVS Pharmacy completed cost-based reimbursement transition across commercial, Medicare, and Medicaid
- Caremark achieved strong customer wins and retention heading into 2026
- Press Ganey awarded Aetna inaugural "Health Plan of the Year" for quality, innovation, and member experience
- Signify Health served 3.5 million consumers with in-home visits, supporting 500,000 reconnections to care
What Did Management Say About PBM Regulation?
CEO Joyner addressed PBM reform head-on, expressing confidence that Caremark's value proposition remains intact.
"The PBM value, we believe, still stays intact. We remain the only entity whose sole job is to create competition and negotiate for lower prices on the pharmaceutical supply chain."
— David Joyner
Brand inflation remains the key issue: In 2026 alone, branded manufacturers made over 750 drug price increases, adding $25 billion of cost to the healthcare system .
Key regulatory positions:
Value creation quantified: CVS generates $280 billion of annual savings for clients and members — $235 billion from Aetna network negotiations and $45 billion from Caremark manufacturer negotiations .
Q&A Highlights
Commercial Membership Strength: Steve Nelson reported commercial membership at 18 million members — the highest level in a decade. Growth driven by better-than-expected retention and "innovative products that resonate with sophisticated purchasers" .
Group MA Repricing: 50% of the group Medicare Advantage block was up for renewal in 2026, and CVS "executed on those rate renewals in a very positive way" .
Medicaid Performance: Business "performing in line with expectations" with a strong year of rate advocacy in 2025. Maintaining cautious outlook in high-trend environment .
Technology Investments: Management discussed the "Open Engagement Platform" initiative announced at Investor Day, with 185 million consumers engaging with CVS Health annually. Product launches and partnership announcements expected in coming quarters .
Rite Aid Integration: Successfully welcomed 9 million new patients and over 3,500 colleagues from Rite Aid. The acquisition expanded CVS's coast-to-coast footprint while serving communities that lost their pharmacy .
Notable One-Time Items
CVS had several significant non-recurring items that impacted comparisons:
The Omnicare subsidiaries filed for Chapter 11 bankruptcy in September 2025, leading to deconsolidation . The related worthless stock deduction provided a $1.9 billion tax benefit .
Legacy litigation charges included $929 million related to Omnicare False Claims Act violations and $291 million for PBM reporting practices .
Balance Sheet and Cash Flow
Full-year cash flow from operations of $10.6 billion was up 17% YoY . However, management guided to reduced cash flow of at least $9.0 billion for 2026 .
Capital expenditures were $2.8 billion for 2025, and dividends paid totaled $3.4 billion .
Historical Performance Trend
*Values retrieved from S&P Global
CVS has now beaten estimates in 6 of the last 8 quarters, showing improved consistency after the challenging Q2-Q3 2024 period.
Looking Ahead: Forward Catalysts
Near-term catalysts to monitor:
- 2027 MA Final Rate Notice — CMS engagement ongoing; final rates could be more favorable than proposed
- Caremark 2026 selling season — Strong customer wins and retention suggest continued PBM growth
- TrueCost adoption — Recent legislation may accelerate client adoption of transparent pricing model
- Open Engagement Platform — Product launches and partnership announcements expected in coming quarters
- Health Care Benefits margin recovery — Management committed to return to target margins; Medicare improvement expected in both 2026 and 2027
Risks:
- 2027 MA rates finalized at inadequate levels despite advocacy
- Medical cost trends remaining elevated across all products
- PBM regulatory changes (though management views as manageable)
- Continued margin pressure in retail pharmacy reimbursement